Prepared by
Dan Henderson, MD, MPH
Anne Carrie, MBA
Abstract
America’s senior population is expected to nearly double over the next thirty years, bringing with it a surge in chronic disease and increasing patient volumes that will place even more strain on an already stressed healthcare system. To stay ahead, health plans and health systems must find smarter, more effective ways to control costs, reduce avoidable care utilization, and support the complex needs of a growing aging population that prefers to live independently at home.
This paper presents findings from research that: (1) examines the care needs, utilization patterns and return on investment (ROI) for Connect America’s personal emergency response system (PERS) subscribers, and (2) evaluates the impact of PERS with the CareSage predictive analytics platform on emergency department utilization, hospitalizations, and overall healthcare costs.
Executive Summary
A growing senior population and rising rates of chronic disease are putting pressure on traditional care models. This shift is accelerating the need for more innovative approaches that keep aging and vulnerable individuals safe, independent, and well-supported at home while improving efficiency and reducing unnecessary costs.
Why it Matters
The U.S. healthcare system is not adequately prepared to meet the complex care needs of a growing elderly population, many of whom prefer to age in place. When seniors lack supports and systems to remain safe at home, a frequent consequence is costly hospital-based care due to illness, much of which is preventable. As a result, unnecessary utilization, rising costs and a lack of resources continue to burden an already strained health system.
Addressing Unnecessary Care: A Multi-Billion-Dollar Problem
Each year, an estimated 18 million avoidable emergency department (ED) visits contribute to billions in unnecessary healthcare spending. Research shows that 30% to 70% of ED visits and hospitalizations are potentially avoidable, representing a critical opportunity for healthcare organizations and health plans to improve care and reduce unnecessary utilization.¹⁻³ By identifying risk, enabling earlier interventions and delivering real-time support in the moment of need, care teams can significantly improve outcomes and lower care costs.
Using PERS to Lower Avoidable ED Utilization
To better understand the care needs and utilization patterns of our more than 900,000 Connect America PERS subscribers, researchers conducted a quantitative data analysis of over 211,000 medical alert calls.
The findings revealed that beyond fall-related incidents, PERS was widely used to signal help in situations associated with chronic conditions, such as pain, respiratory distress, diabetic reaction, and cardiac-related symptoms. Most significantly, nearly half of all subscribers received on-site assistance without needing emergency transport, contributing to an estimated $236 million reduction in potentially avoidable care costs.
To determine the impact of PERS with the CareSage analytics platform and tailored interventions on ED utilization, readmission rates and hospitalization costs, researchers at Massachusetts General Hospital and Harvard Medical School conducted an IRB-approved study on over 370 subscribers. The results from this study demonstrated meaningful reductions in readmissions, ED transfers, and a 31% decrease in hospitalization costs.
Introduction
America is aging. Every day, more than 10,000 people turn 65 — a number that is expected to more than double by 2050.⁴ Americans are also living longer than ever before. While the average life span expectancy is increasing, many individuals are spending more of those years burdened by disease and disability.⁵
While aging in and of itself is not a disease, it significantly increases the risk of developing chronic illnesses. Nearly 80% of all seniors in the U.S. live with one or more chronic illness, including diabetes, COPD, heart disease and arthritis. These conditions often bring challenges, including physical limitations, chronic pain, and an increased risk of falls. All of which can threaten independence, diminish quality of life and increase reliance on healthcare services.⁶⁻⁷
Chronic disease and the rising costs of care
 Chronic disease places a tremendous burden on the U.S. healthcare system — a burden that will continue to grow as the Baby Boomer generation ages and the number of individuals with chronic illnesses increases.
Chronic disease places a tremendous burden on the U.S. healthcare system — a burden that will continue to grow as the Baby Boomer generation ages and the number of individuals with chronic illnesses increases.
According to the Centers for Disease Control and Prevention (CDC), 90% of America’s $3.8 trillion annual healthcare expenditures are for patients with chronic and mental health conditions.⁸
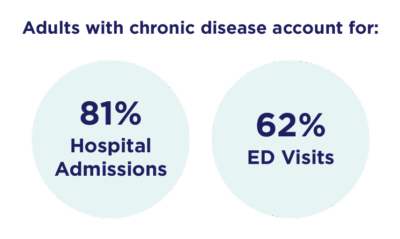
Adults with chronic conditions drive higher utilization and costs, and account for 81% of hospital admissions and 62% of ED visits.¹⁰⁻¹¹
Addressing preventable hospitalizations and ED utilization
According to the Agency for Healthcare Research and Quality (AHRQ), a substantial share of emergency department (ED) visits and hospitalizations in the U.S. are preventable. In 2017 alone, potentially avoidable adult inpatient stays accounted for $33.7 billion in hospital costs. Research further suggests that 30% to 70% of ED visits and hospitalizations could be avoided.¹⁻³ These preventable events are especially common among older adults and are more likely in lower-income communities, highlighting the need for more proactive care strategies.¹³
Delivering earlier interventions and real-time support with PERS
To better support the complex needs of aging and vulnerable populations and help lower avoidable care costs, many healthcare organizations have adopted connected care technologies such as PERS. While PERS are commonly known for providing emergency response and fall detection services, their value extends far beyond falls. Connect America’s PERS provides access to a broad range of services such as:
- 24/7 real-time emergency support
- Multimodal monitoring, including tracking activity, movement, falls and wandering
- Concierge-level customer service
- Clinical triage by registered nurses
- Family and caregiver event notifications
- Support for social needs
Connect America’s PERS monitoring technology and services support individuals in their moment of need and can be used to signal for help for a broad range of emergent and non-urgent situations, such as:
Medical Emergencies:
- A cardiac event
- Difficulty breathing
- Severe pain
- A fall
- Complications from chronic conditions
Non-Medical Situations:
- Inability to get up
- Safety concerns
- Assistance reaching a loved one
- Help scheduling a doctor’s appointment
- Loneliness
Whether it’s a fall, a medical issue, or a moment of uncertainty, these services provide peace of mind and a bridge to timely support and care. During the pandemic, PERS helped care teams identify COVID-related symptoms early, enabling timely provider intervention and reducing ED and ICU admissions.¹² Beyond emergencies, PERS support post-discharge monitoring to help prevent readmissions while also offering a response option for lower-acuity issues.
PERS combined with clinical triage (PERS+) allows care teams to leverage inbound alerts to ensure individuals get the appropriate level of care — enabling clinically guided interventions that prevent unnecessary ED visits and improve both clinical outcomes and cost efficiency.
PERS with CareSage Predictive Analytics
Connect America’s PERS captures critical data from inside the home, tracking incidents such as falls, respiratory distress, chest pain, or general pain, as well as other check-in or social calls for a more complete view beyond clinical settings. Such events may indicate a decline in status which may be captured earlier with PERS – enabling quicker interventions.
When paired with the CareSage predictive analytics platform, this solution helps care teams identify high-risk patterns in activity and mobility, enabling more effective risk management for patient and member populations.
PERS subscriber event analysis
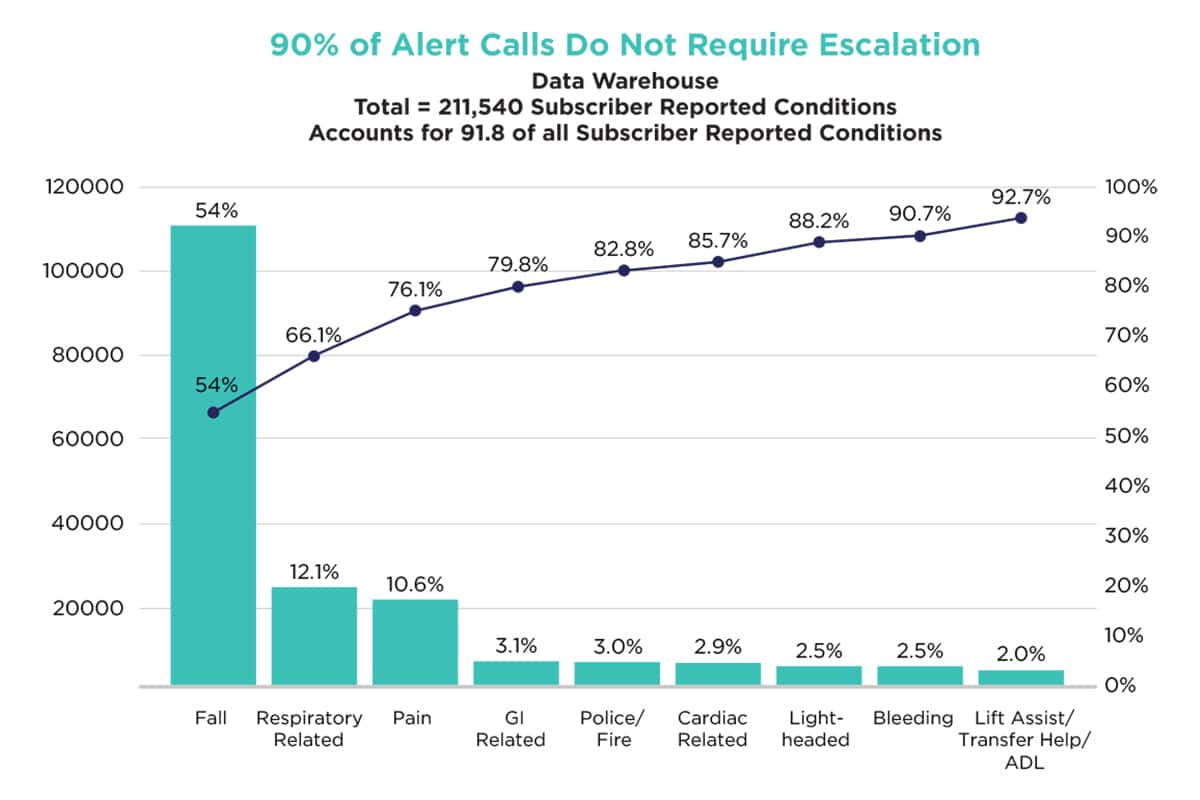
To better understand the care needs and utilization patterns of our more than 900,000 subscribers, we conducted a qualitative data analysis of more than 211,000 alert calls from our PERS subscribers. Our researchers reviewed subscriber events, most common symptoms and the action taken to provide the appropriate care response. In addition, we examined the emergency medical service call dispatch outcomes to determine the number of events addressed onsite vs. events transported.
Study design, methods and results
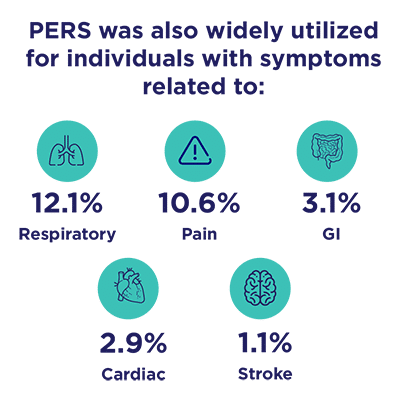 Our methods of analysis were labor-intensive across call centers. The results showed that while falls were attributed to 53% of the alert calls, PERS was also widely utilized for individuals with symptoms related to:
Our methods of analysis were labor-intensive across call centers. The results showed that while falls were attributed to 53% of the alert calls, PERS was also widely utilized for individuals with symptoms related to:
- 12.1% Respiratory
- 10.6% Pain
- 3.1% GI
- 2.9% Cariac
- 1.1% Stroke
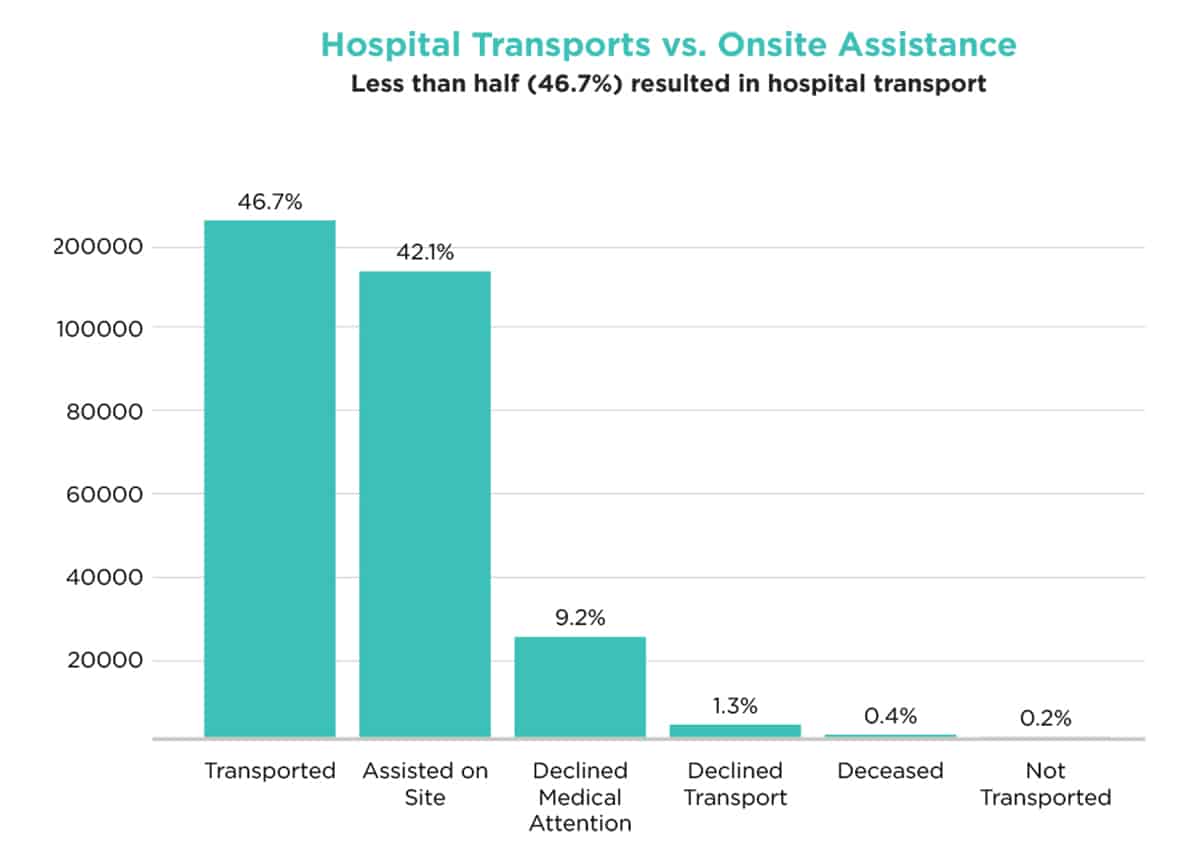
Additionally, nearly 90% of all subscriber alert calls did not require escalation to higher levels of care. In fact, a significant number of cases, 42.1% or 113,547 adult subscribers, were assisted with their care needs onsite without emergency intervention or hospitalization. Our analysis used national averages to estimate potentially avoided ED and hospitalization costs for these subscribers, resulting in an estimated cost savings of $236 million and an annual ROI of approximately 3.3:1. (for every $1 invested, $3.30 was saved)
Reducing readmissions, ED utilization and healthcare costs
To demonstrate the impact of PERS paired with the CareSage analytics platform and tailored interventions on ED utilization, readmissions rates and hospitalization costs, researchers at Massachusetts General Hospital and Harvard Medical School conducted an IRB-approved study of over 370 randomized participants, including 189 (controlled group) and 181 (intervention group).
Early interventions with PERS improve outcomes and lower hospitalization and ED utilization costs
The results showed a meaningful reduction in healthcare utilization and costs including a 68% decrease in 90-day readmissions with a corresponding triple decrease of proportion in patients with any 90-day readmission, a 53% decrease in 180-day readmissions, a 49% decrease of 180-day EMS encounters, and a 31% decrease in hospitalization costs.¹³
Study Results*
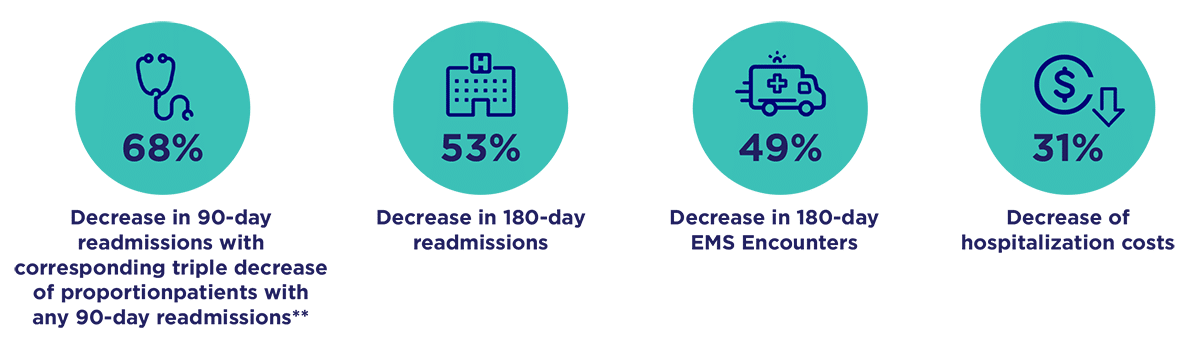
* Statistically significant outcomes (p<0.05 using intention-to-Treat approach
** 10.4% control vs. 3.1% intervension group
Nikolova-Simons M. Bersche Golas S, op den buijs J Palacholla RS. Gerberg G, Orenstein A. Kvedar J. (3rd June 2021). A randomized trial examining the effect of predictive analytics and tailored interventions on the cost of care. npj Digit. Med 4, 92 (2021). http://doi.org/10.1038/s41746-021-00449-w
Bersche Golas S. Nikolova-Simons M. Palacholla R. op den Buijs
J. Garberg O. Orenstein A. Kvedar J. (10th June 2021) Predictive analytics and tailored interventions improve clinical outcomes in older adults: a randomized controlled trial. npj Digit. Med 4, 97 (2021). https://doi.org/10.1038/s41746-021-00449-w
Conclusion
As healthcare costs rise and the need for home- based support becomes more urgent, payers and providers must find smarter, more efficient ways to meet the complex care needs of aging and vulnerable populations.
This white paper demonstrates Connect America’s PERS is a valuable, cost-effective solution that helps address emergent and non- emergent care needs in real time. By enabling timely interventions, PERS can help prevent complications from escalating, resulting in measurable reductions in emergency care utilization and hospitalizations. This proactive model enhances efficiency, reduces avoidable costs, and most importantly, supports the safety, health, and independence of those who prefer to age gracefully at home.
Download a Copy
To download a complete copy of this white paper, please click here.
References
- Khullar D, Zhang Y, Kaushal Potentially Preventable Spending Among High-Cost Medicare Patients: Implications for Healthcare Delivery. J Gen Intern Med. 2020 Oct;35(10):2845-2852. doi: 10.1007/s11606-020-05691-8. Epub 2020 Feb 26. PMID: 32103440; PMCID: PMC7573047.
- United Health Group. (July, 2019) 18 Million Avoidable Hospital Emergency Department Visits Add $32 Billion in Costs to the Health Care System Each https://www.unitedhealthgroup.com/content/dam/UHG/PDF/2019/UHG-Avoidable-ED-Visits.pdf
- Agency for Healthcare Research and Quality. (2020, June). Statistical Brief #259, Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality. https://hcup-us.ahrq.gov/reports/statbriefs/sb259-Potentially-Preventable-Hospitalizations-2017.jsp
- National Center for Health Statistics. (2021, August 3). Older Persons’ Health. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/fastats/older-american-health.htm
- Medina, , Sabo, S., Vespa, J. (2020, February). Living Longer: Historical and Projected Life Expectancy in the United States, 1960 to 2060. United States Census Bureau, Population Estimates and Projections Current Population Reports. https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1145.pdf
- Osborn, , Doty, M., Moulds, D., Sarnak, D., Dana, O., Shah, A. (2017). Older Americans were Sicker and Faced More Financial Barriers to Health Care than Counterparts in Other Countries. 2017 Commonwealth Fund International Health Policy Survey of Older Adults. https://www.healthaffairs.org/doi/full/10.1377/hlthaff.2017.1048
- National Center for Chronic Diseases Prevention and Health Chronic Disease in America. Centers for Disease Control and Prevention. https://www.cdc.gov/chronic-disease/data-research/facts-stats/index.html
- National Council on (2021, January 1) Get the Facts on Healthy Aging. National Council on Aging. https://www.ncoa.org/article/get-the-facts- on-healthy-aging
- Centers for Disease Control and (2021). CDC Health and Economic Costs of Chronic Diseases. National Center for Chronic Disease Prevention and Health Promotion. https://www.cdc.gov/chronic-disease/data-research/facts-stats/?CDC_AAref_Val=https://www.cdc.gov/chronicdisease/about/costs/index.htm
- Partnership to Fight Chronic Disease. The Growing Crisis of Chronic Disease in the US. https://commed.vcu.edu/Chronic_Disease/2008/ChronicDiseaseFactSheet.pdf
- QuickStats: Distribution of Emergency Department Visits Made by Adults, by Age and Number of Chronic Conditions — United States, 2017–2019. MMWR Morb Mortal Wkly Rep 2022;71:33. DOI: http://dx.doi.org/10.15585/mmwr.mm7101a6
- Phillion, , (2021, November 22). Improving Remote Monitoring to Care for Isolated Seniors. PSQH Patient Safety and Quality Healthcare. https://www.psqh.com/analysis/improving-remote-monitoring-to-care-for-isolated-seniors/
- Nikolova-Simons, M., Golas, S.B., den Buijs, J.o. et al. A randomized trial examining the effect of predictive analytics and tailored interventions on the cost of care. npj Digit. Med. 4, 92 (2021). https://doi.org/10.1038/s41746-021-00449-w

