Rosemary Kennedy, Ph.D., RN, MBA, FAAN
Anne Carrie, MBA
Abstract
America’s senior population is projected to nearly double over the next thirty years, which will result in higher rates of chronic disease and rising patient volumes, further increasing demand on an already stressed healthcare system. For healthcare organizations seeking solutions that help reduce hospitalizations, lower care costs, and extend quality of life, connective health technologies such as personal emergency response systems (PERS) have been shown to make a significant impact.
This paper reviews the outcomes of two research studies conducted to measure the impact of Connect America’s PERS with CareSage analytics on emergency department (ED) utilization, hospitalizations, and overall healthcare costs.
Executive Summary
As the U.S. healthcare industry continues to face increasing rates of chronic disease and a growing senior population, the ability to deliver efficient, quality care while lowering costs requires the adoption of new and innovative care delivery models.
Connective care technologies offer a cost-effective solution to help healthcare organizations reduce unnecessary care utilization while enabling vulnerable senior populations to remain safely in their homes.
For example, Connect America’s PERS with CareSage provides payers and providers with actionable insights that prompt earlier interventions for more proactive care of aging populations. By delivering a continuous line of sight into an individual’s health status and well-being, PERS with CareSage helps identify at-risk patients before a need arises, resulting in fewer hospitalizations and better outcomes.
To measure the impact that PERS with CareSage analytics has on healthcare utilization and to better understand the care needs of our more than 900,000 Connect America PERS subscribers, we conducted a quantitative data analysis of over 211,000 medical alert calls.
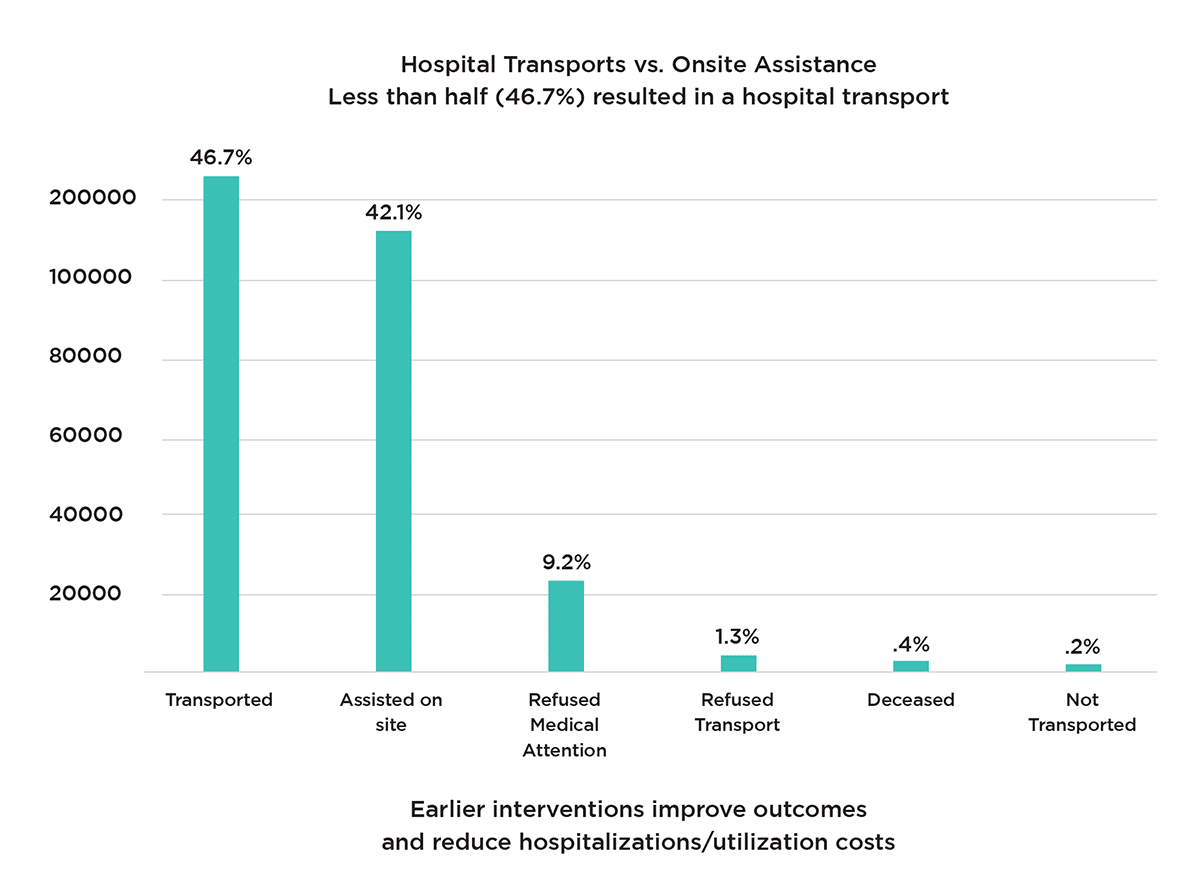
The data collected from this research showed that in addition to falls, PERS with CareSage was widely used to signal for help in situations associated with chronic conditions such as pain, respiratory distress, diabetic reaction, and cardiac-related symptoms. More importantly, nearly half of subscribers were able to be assisted on-site without requiring emergency transport or hospitalization.
To determine the value of PERS with CareSage and its impact on ED utilization, readmission rates and hospitalization costs, we conducted an IRB-approved study on over 370 randomized subscribers. The results from this study demonstrated significant reductions in readmissions, ED visits and overall hospitalization costs.
Introduction
America is aging. Every day more than 10,000 people will turn 65, and this number will double in the next few decades.¹ Americans are also living longer than ever before. According to the U.S. Census, life expectancy is projected to increase by about six years, from 79.7 in 2017 to 85.6 in 2060.²
While aging in and of itself is not a disease, it is a major risk factor for developing chronic disease. Nearly 80% of all seniors in the U.S. live with one or more chronic diseases. Aging adults with conditions such as diabetes, COPD, heart disease and arthritis are exacerbated by physical limitations, pain, falls and other adverse events. All of which can result in the loss of independence, reduced quality of life and a greater reliance on healthcare services.³⁻⁵
Chronic disease and the rising costs of care
The management of chronic diseases presents a tremendous burden on the U.S. healthcare system that will continue to grow as the Baby Boomer generation ages and the number of individuals with chronic diseases increases.
The Centers for Disease Control and Prevention (CDC) estimates that 90% of America’s $3.8 trillion annual healthcare expenditures are for patients with chronic and mental health conditions.⁶
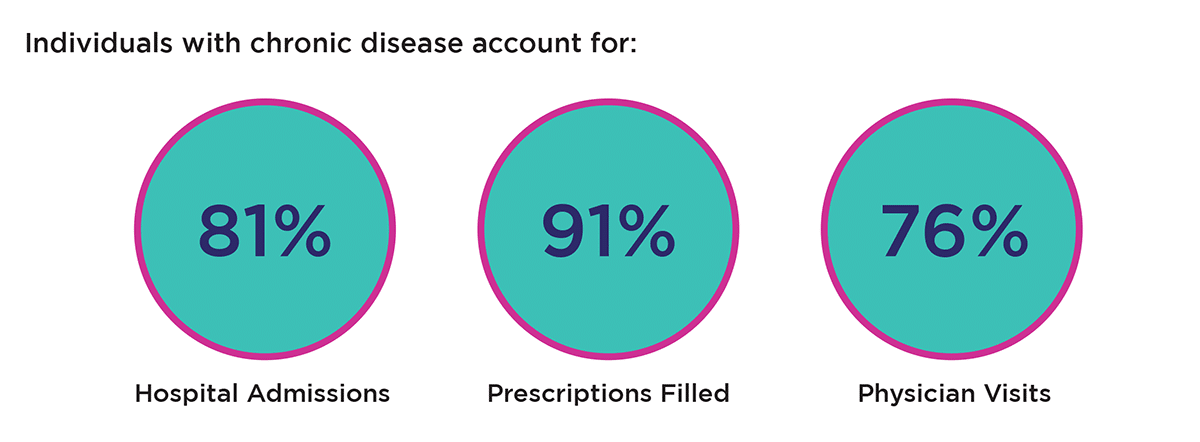
Healthcare utilization and costs for individuals with chronic conditions are more than twice as much as those without, and their hospitalization rates are nearly four times higher. They are among the largest users of healthcare services, accounting for 81% of hospital admissions, 91% of all prescriptions filled, and 76% of all physician visits.⁷
Addressing preventable hospital admissions and ED visits with PERS
 Because the U.S. healthcare system is fragmented and not adequately designed to meet the growing needs of an expanding elderly population with chronic conditions, this often leads to unnecessary usage and medical costs. According to the Agency for Healthcare Research and Quality (AHRQ), there were approximately 3.5 million potentially preventable adult inpatient stays that accounted for $33.7 billion in 2017. The majority of potentially avoidable stays (77.1%) and associated costs were for individuals with chronic conditions.⁸
Because the U.S. healthcare system is fragmented and not adequately designed to meet the growing needs of an expanding elderly population with chronic conditions, this often leads to unnecessary usage and medical costs. According to the Agency for Healthcare Research and Quality (AHRQ), there were approximately 3.5 million potentially preventable adult inpatient stays that accounted for $33.7 billion in 2017. The majority of potentially avoidable stays (77.1%) and associated costs were for individuals with chronic conditions.⁸
In an effort to reduce unnecessary care utilization to help better support vulnerable senior populations, many healthcare organizations have implemented the use of connective health technologies such as personal emergency response services (PERS).
While PERS are most often known for providing fall detection services for seniors who wish to live independently at home, PERS are for more than just falls. PERS technology can also be used to signal for help in emergency situations such as a cardiac event, difficulty breathing, pain or the worsening of a chronic condition.
Throughout the pandemic, the use of PERS has played a critical role in identifying COVID-related symptoms for subscribers early on, enabling providers to intervene before their patients’ conditions deteriorated and they were forced to the ED or ICU.⁹
The technology has also been effective for post-care monitoring after patients are treated, discharged from the hospital and back in their homes. Post-care monitoring is a significant factor in reducing unnecessary readmissions while ensuring the best possible outcomes for patients. In addition, PERS can provide a response to lower acuity symptoms, helping to reduce the strain on emergency care services. Finally, PERS provide subscribers with a social benefit. Feelings of loneliness and social isolation are common among seniors living at home and can significantly affect health and well-being. PERS can offer a human element by providing the ability to connect to a live person and hear a friendly voice that can offer help or support.
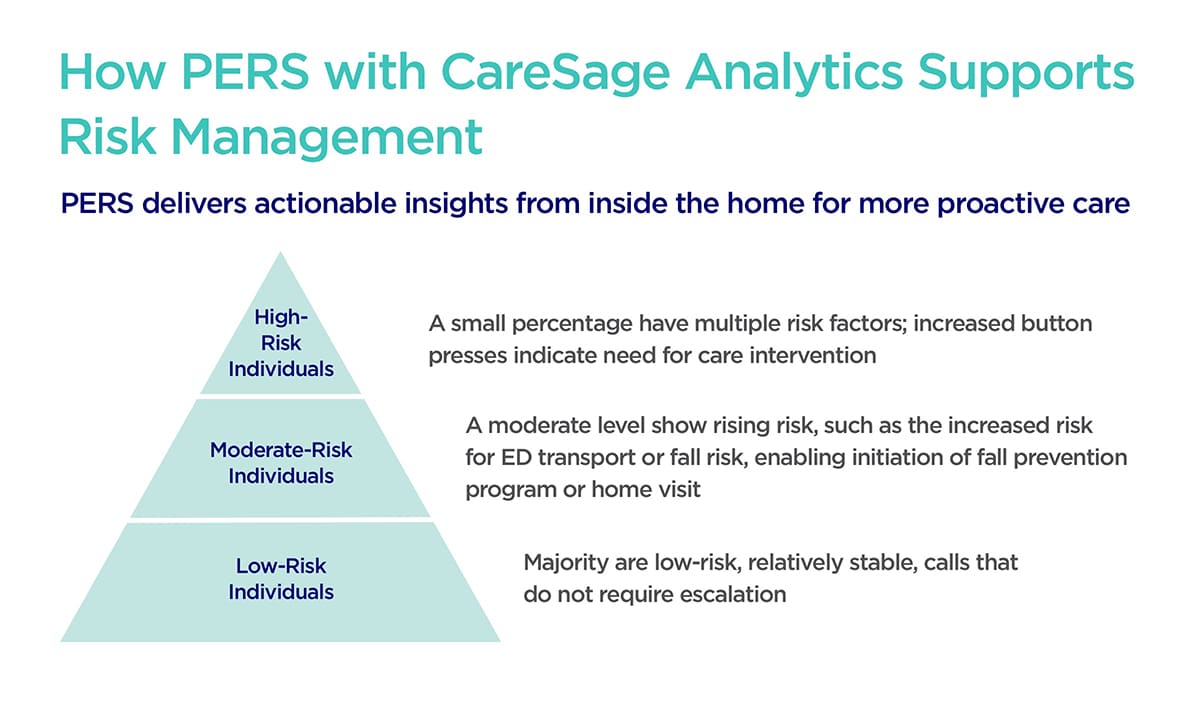
Yet, some PERS can go a step further. To more efficiently manage care utilization, healthcare organizations, case managers and clinicians need better insight into their patient’s health beyond the four walls of the healthcare system. Connect America’s PERS with CareSage analytics helps payers and providers identify high-risk individuals by providing a continuous line of sight into the home to help facilitate earlier interventions that are essential for cost containment and outcomes.
Connect America’s PERS with CareSage analytics
 Connect America’s PERS with CareSage analytics collects patient data while they are at home, in their natural environment. This information includes the time stamp, type, situation, and outcome—of incidents such as falls, respiratory issues, chest pain, or general pain, as well as other check-in or social calls. Such events may indicate a decline in patient status which may be captured earlier with PERS – enabling quicker interventions and reducing the risk of hospital transports or admissions, as demonstrated below.
Connect America’s PERS with CareSage analytics collects patient data while they are at home, in their natural environment. This information includes the time stamp, type, situation, and outcome—of incidents such as falls, respiratory issues, chest pain, or general pain, as well as other check-in or social calls. Such events may indicate a decline in patient status which may be captured earlier with PERS – enabling quicker interventions and reducing the risk of hospital transports or admissions, as demonstrated below.
PERS subscriber event analysis
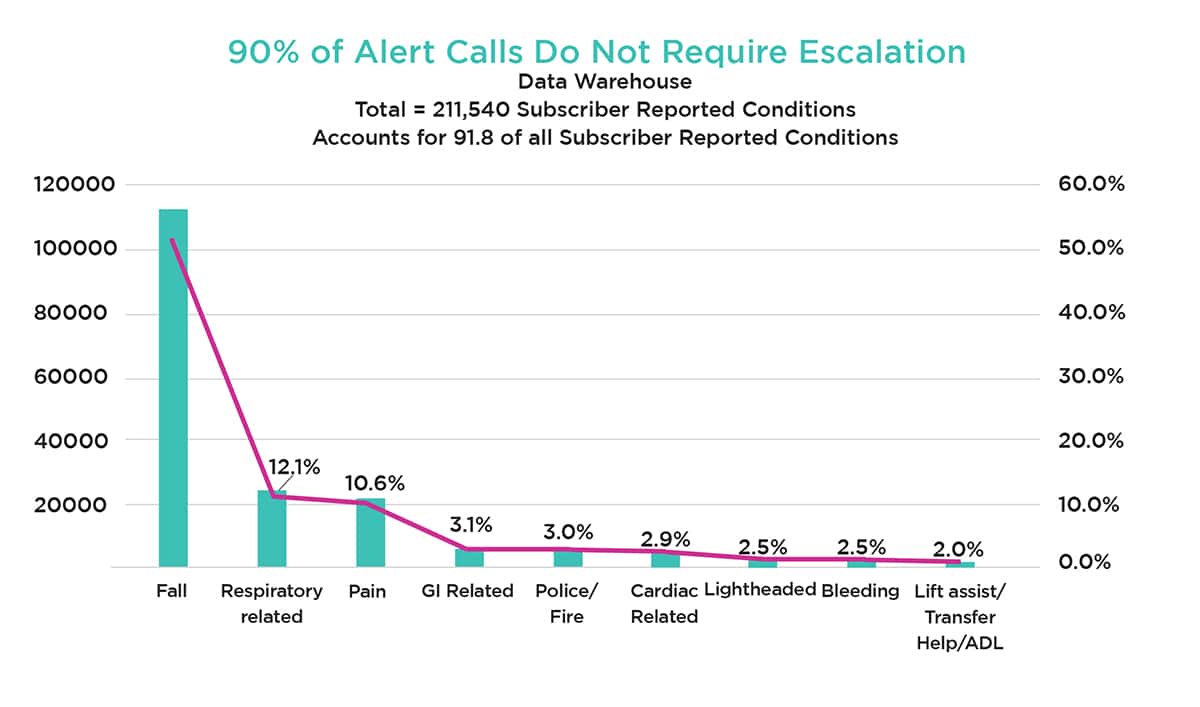
To measure the value of Connect America’s PERS with CareSage analytics and better understand the care needs of our more than 900,000 subscribers, we conducted a qualitative data analysis of more than 211,000 alert calls from our PERS subscribers. We reviewed subscriber events, most common symptoms and the action taken to provide the appropriate care response. In addition, we examined the emergency medical service call dispatch outcomes to determine the number of events addressed onsite vs. events transported.
Study design, methods and results
Our methods of analysis were labor-intensive secondary to underlying variation in terminology across the call centers. The data collected from this study suggests that falls attributed to just 53% of the alert calls. PERS was widely utilized for individuals with respiratory (12.1%), pain (10.6%), GI (3.1%), cardiac (2.9%) and stroke (1.1%) related symptoms.
The analysis showed that nearly 90% of all subscriber alert calls did not require escalation to higher levels of care. In fact, in a significant number of cases 42.1% or 113,547 adult subscribers were able to be assisted with their care needs resolved onsite without emergency intervention or hospitalization and less than half resulted in hospital transport.
The Impact of PERS: Reducing readmissions, ED utilization and hospitalization costs
In an effort to better understand and demonstrate the impact of PERS with CareSage on ED utilization, readmissions rates and hospitalization costs, we conducted IRB approved research study of over 370 randomized individuals, including 189 (controlled group) and 181 (intervention group). Researchers evaluated the impact of PERS with CareSage analytics and tailored interventions on the healthcare utilization of mid-acuity adults. In addition, we assessed the impact on ED utilization costs and readmission rates.
The study results showed a significant reduction in readmissions, ED visits and overall hospitalization costs, including a 68% decrease in 90-day readmissions with a corresponding triple decrease of proportion in patients with any 90-day readmission, a 53% decrease in 180-day readmissions, a 49% decrease of 180-day EMS encounters, and a 31% decrease in hospitalization costs.
Study Results*

* Statistically significant outcomes (p<0.05 using intention-to-Treat approach
** 10.4% control vs. 3.1% intervention group
Nikolova-Simons M. Bersche Golas S, op den buijs J Palacholla RS. Gerberg G, Orenstein A. Kvedar J. (3rd June 2021). A randomized trial examining the effect of predictive analytics and tailored interventions on the cost of care. npj Digit. Med 4, 92 (2021). http://doi.org/10.1038/s41746-021-00449-w
Bersche Golas S. Nikolova-Simons M. Palacholla R. op den Buijs J. Garberg O. Orenstein A. Kvedar J. (10th June 2021) Predictive analytics and tailored interventions improve clinical outcomes in older adults: a randomized controlled trial. npj Digit. Med 4, 97 (2021). https://doi.org.10.1038/s41746-021-00463-y
Conclusion
For healthcare organizations seeking solutions that help lower care costs and enable aging seniors to live more independently in their homes, connective health technologies such as Connect America’s PERS are a proven and reliable investment.
Connect America’s PERS with CareSage enables healthcare organizations to quickly identify high-risk individuals and facilitate more preventative interventions that enhance efficiency, care and outcomes. Payers and providers benefit from higher satisfaction, increased quality, reduced clinician workload, and lower care costs. At the same time, seniors experience more seamless care coordination, fewer hospitalizations, better overall health, and the ability to age gracefully and well in their homes.
To download a complete copy of this white paper, please click here.
References
- National Center for Health Statistics. (2021, August 3). Older Persons’ Health. Centers for Disease Control and Prevention. https://www.cdc.gov/nchs/fastats/older-american-health.htm
- Medina, L., Sabo, S., Vespa, J. (2020, February). Living Longer: Historical and Projected Life Expectancy in the United States, 1960 to 2060. United States Census Bureau, Population Estimates and Projections Current Population Reports. https://www.census.gov/content/dam/Census/library/publications/2020/demo/p25-1145.pdf
- Osborn, R., Doty, M., Moulds, D., Sarnak, D., Dana, O., Shah, A. (2017). Older Americans were Sicker and Faced More Financial Barriers to Health Care than Counterparts in Other Countries. 2017 Commonwealth Fund International Health Policy Survey of Older Adults. https://www.commonwealthfund.org/publications/journal-article/2017/nov/older-americans-were-sicker-and-faced-more-financial-barriers
- National Center for Chronic Diseases Prevention and Health Promotion. Chronic Disease in America. Centers for Disease Control and Prevention. https://www.cdc.gov/chronicdisease/resources/infographic/chronic-diseases.htm
- National Council on Aging. (2021, January 1) Get the Facts on Healthy Aging. National Council on Aging.https://www.ncoa.org/article/get-the-facts-on-healthyaging
- Centers for Disease Control and Prevention. (2021). CDC Health and Economic Costs of Chronic Diseases. National Center for Chronic Disease Prevention and Health Promotion. https://www.cdc.gov/chronicdisease/about/costs/index.htm
- Partnership to Fight Chronic Disease. The Growing Crisis of Chronic Disease in the US. https://www.fightchronicdisease.org/sites/default/files/docs/Growing-
CrisisofChronicDiseaseintheUSfactsheet_81009.pdf - Agency for Healthcare Research and Quality. (2020, June). Statistical Brief #259, Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality. https://www.hcup-us.ahrq.gov/reports/statbriefs/sb259-Potentially-Preventable-Hospitalizations-2017.jsp
- Phillion, M., (2021, November 22). Improving Remote Monitoring to Care for Isolated Seniors. PSQH Patient Safety and Quality Healthcare. https://www.psqh.com/analysis/improving-remote-monitoring-to-care-for-isolated-seniors/

